Fungal Nails occur in around 8% of the population in the
UK
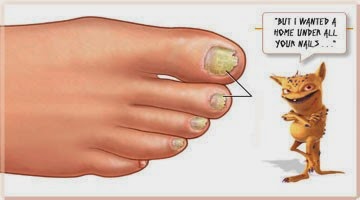
There are different types of infection, or onychomycosis, but
by far the most common is that which is caused by fungi tracking from the skin of the foot.
It starts at the end of the nail and moves
back towards the 'half moon' leaving yellow or brown patches and streaks as it
progresses. The nail is very crumbly
when it is cut and may have a bad odour.
Another type invades the top of the nail plate directly
and causes a white, pitting effect. Less common variations can cause complete destruction of the nail
matrix, but it is worth remembering that any one person can display a combination of all
types and once one nail becomes infected, it can easily spread to the others.
Any fungus likes a warm, dark and
moist environment and, these are the conditions you offer your feet when they
are constantly encased in footwear. Of
course, the fungus needs to be present in the first instance , but it can be
easily picked up from other warm and moist areas such as swimming pool changing
areas and shower rooms. Once present, a fungus can survive in footwear for up to six months. It usually enters the
skin through small cuts or through small
separations between the nail and the nail bed.
People with poor circulation, those with
diabetes and those with a weakened immune system should take extra care as they
are more vulnerable to fungal nail infections.
Two dermatophytes are responsible
for around 90% of all fungal infections. Trichophyton
rubrum is usually responsible for
the fungus which progresses from the end of the nail towards the half moon,
whereas Trichophyton mentagrophytes is more often associated with the superficial
white areas attacking the nail plate. An infection which starts at the 'half
moon' moving towards the free edge is usually caused by non-dermatophyte
moulds.
At first, a fungal infection will
probably not cause any problems other than cosmetic changes in the nail, but it
is possible that in severe cases they can become very uncomfortable and
even painful as the nail thickens and
causes inflammation of the nail bed.
Treatment can be topical or
systemic or both. There are obvious problems associated with any systemic
medication and so the first line of treatment is usually topical. As the nail
has a very hard top layer, it is advisable to file the nail to enable the
antifungal agent to penetrate the nail plate more easily. Research has also found that applying a urea
cream to the nail prior to the antifungal lacquer, allows for better
penetration and better results.
 Progress of any treatment is slow. As a
toenail grows on average 1.5 - 2mm per month, it can be disheartening when
there appears to be little improvement after diligent treatment. It is important to recognise that the affected
part of the nail will not improve in
appearance, but as the yellow and white areas grow and are cut away, new growth
should look nice
and clear. Complete resolution can take around a year to eighteen months.
Progress of any treatment is slow. As a
toenail grows on average 1.5 - 2mm per month, it can be disheartening when
there appears to be little improvement after diligent treatment. It is important to recognise that the affected
part of the nail will not improve in
appearance, but as the yellow and white areas grow and are cut away, new growth
should look nice
and clear. Complete resolution can take around a year to eighteen months.
Perseverance is
paramount. Application of the treatment must be carried out every day, preferably
twice a day; alongside allowing the feet to breathe without permanently wearing
occlusive footwear.
New therapies are
becoming more widely available, such as laser treatment and aromatherapy
products.
Body Essentials have
developed an aromatherapy product for the treatment of fungal nails, Nourish
Your Nails. This has been well reviewed and is definitley worth trying. If
your nails are yellowed or if you think you may have a fungal infection in your
nails, Nourish your Nails will gently lighten and brighten the nail plate.






